Those who have been in Kinomatic’s virtual reality environment and have examined a patient model know the value and potential that virtual reality technology has in the medical setting. Everything from medical training, to surgical planning, and perhaps one day even intraoperative applications, virtual reality technology is rapidly weaving its way into the fabric of healthcare. It’s always nice to read about how other researchers are experimenting and utilizing 3D virtual reality technology to improve accuracy and postoperative outcomes. We came across an article published in 2010 where researchers were using an early version of a virtual reality-style system using haptic feedback in order to plan pelvic fracture surgeries.
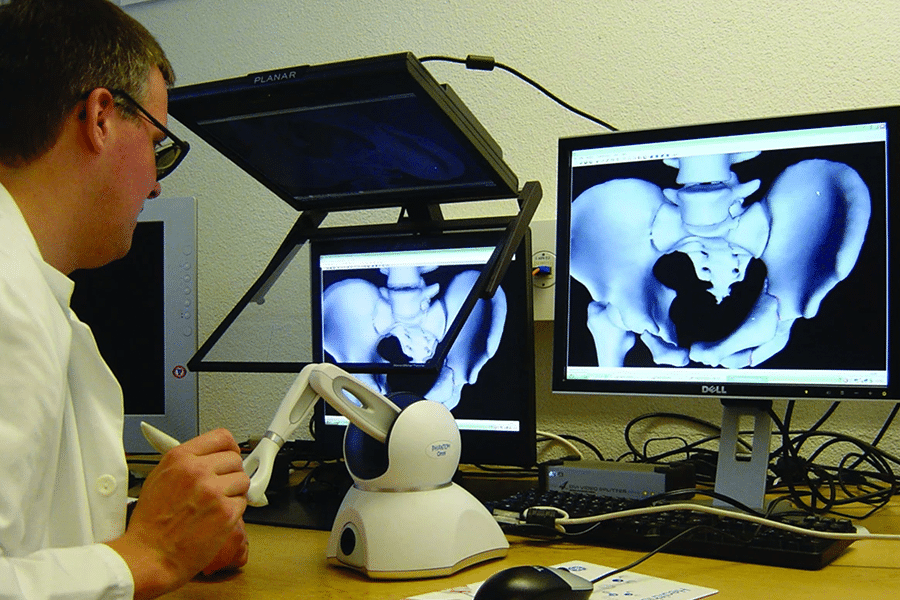
In 2010 the virtual reality headsets that we know of today were likely just in the development and prototype phase. Therefore, when talking about the “virtual reality” system used in this study, don’t think of headsets, but rather 3D models manipulated on a 2D screen. The cool thing about this study is the implementation of the haptic feedback through a PHANTOM Omni Developer Kit. The 3D models were created from a CT scan and semiautomatic segmentation of the pelvic bones and bone fragments. Once the model was generated it was viewed on a computer screen and the user could manipulate the pelvic bones and fragments using the haptic feedback arm allowing them to drag and rotate them into the correct anatomical position. When moving the various pieces of the 3D model, the forces resulting from collisions were registered through the haptic device giving the user interactive, tactile feedback.
They found that compared to a standard mouse interface, the haptic feedback device gave them a much more intuitive and direct manipulation of the fracture fragments. Overall, they found that the tool provided quick and reliable virtual fracture reduction stating, “interactive manipulation of the fracture fragments gave the surgeon insight into their spatial relation and helped in choosing the operative side.” They also concluded that the virtual planning significantly helped the surgeon understand the fracture morphology leading to more accurate and efficient reductions.
There are definitely some differences between the system used in the article and how virtual reality surgical planning is done now. Virtual reality technology of today allows for a fully immersive 3D perspective of pre-operative surgical plans. The added benefit of seeing patient anatomy in 3D space allows for even greater spatial familiarity that simply cannot be achieved to the same degree through any other means. The researchers in this study did have something currently not found in most virtual reality systems which is the advanced haptic feedback feature. This is certainly something we can see becoming more ubiquitous to virtual reality systems very soon since the advancements in image clarity and resolution are already exceptional.
These researchers were pushing the boundaries of medical technology more than ten years ago, and still 3D surgical planning for orthopedic surgeries is not done in the majority of practices. Kinomatic is devoted to improving patient outcomes through expanding the use of advanced 3D and virtual reality technology to medical practitioners throughout the country.
To read more about Kinomatic technologies, follow this link.
To read the full article mentioned in this post click here.
Original Article Credit:
Fornaro, J., Keel, M., Harders, M. et al. An interactive surgical planning tool for acetabular fractures: initial results. J Orthop Surg Res 5, 50 (2010). https://doi.org/10.1186/1749-799X-5-50