Manual Total Knee Arthroplasty: Not Taken Over by Robots Yet
An Insight into The Comparison of Manual Total Knee Arthroplasty with Robotic Knee Arthroplasty
In cases of painful degenerative joint degeneration of the knee, total knee arthroplasty (TKA) is the therapy of choice. In the United States alone, there are over 600,000 TKAs conducted each year, and this number is expected to rise to 935,000 by the year 2030. Although TKA has a high success rate, as much as 20% of patients may be unhappy with the results. This might be due to a combination of variables, such as patient expectations and technological issues. Short-term and long-term success rates for TKA patients have increased when the joint is aligned and soft tissues are in balance.
Manual TKA has been in practice for decades. Alignment and balance in a manually performed TKA (MTKA) are achieved mostly through tactile cues and the surgeon’s level of competence and training.
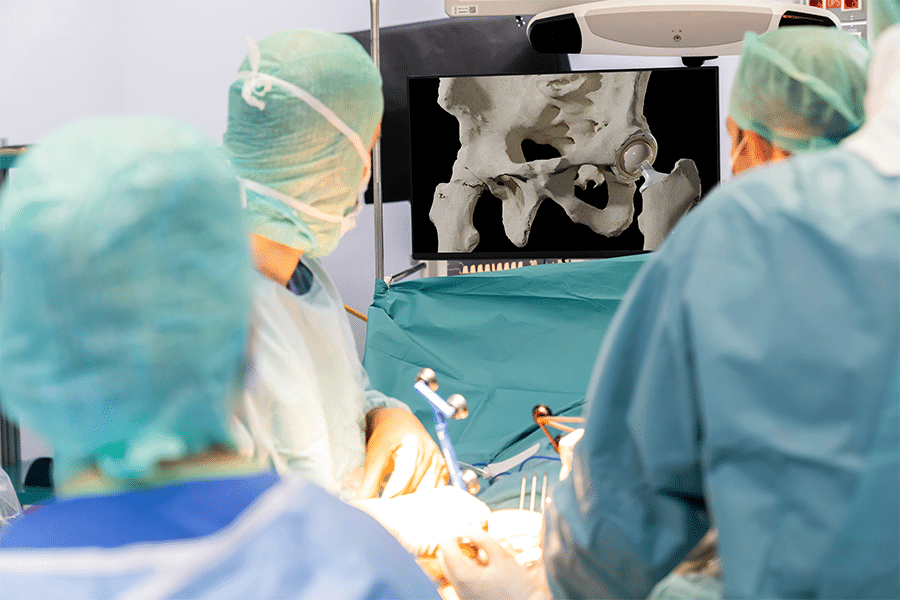
To improve the precision and consistency of bone cutting and ligament balancing, robotics have been incorporated into TKA (RTKA). The most popular system now generates an operation plan using a three-dimensional knee model based on a computed tomography (CT) scan taken before surgery. The robotic arm directs the saw within stereotactic constraints to carry out the strategy and attain alignment and soft tissue balance during surgery.
There is no shortage of literature comparing the two methods of TKA. RTKA has been deemed superior by quite a few studies1. The chief argument is that RTKA is linked to decreased soft tissue trauma2 and a better ligament balance3.
However, there is no extensive data available regarding the long-term outcomes compared to the MTKA. Short-term benefits have been reported, but the added costs have caused a problem.
TKA costs are expected to rise with the advent of automation. When calculating the cost of robotic surgery, it is important to account for the initial investment in the robot and any ongoing maintenance fees. A study published in 2022 comparing the operative times of RTKA versus MTKA concluded that the former took more time. The most significant change was a 32-minute increase in time spent in the operating room4. RTKA procedure also took 8 minutes longer than the traditional one. Sodhi et al. in 2018 showed that surgical time for RTKA and MTKA was time neutral5. However, the preoperative set-up time for the robot and other equipment made RTKA a longer operation. RTKA has been predicted to boost efficiency in the operating room, but this effect was not observed in the study by Tompkins4. This study also showed that the median total cost of RTKA was $2941 more per case than that of MTKA. This included larger supply expenses for RTKA (+$1199), which were mostly attributed to the purchase of the robot, and greater labour costs for RTKA (+$536), which were primarily incurred in the operating room due to lengthier in-room/out-of-room intervals.
Studies advocating the benefits of RTKA suggest that once a good number of surgeons and the Operating room (OR) staff are thoroughly familiarized with the robotic equipment, the efficiency inside the OR will increase and lead to the procedure being more cost-effective.
Similarly, it is a well-established fact that robotic TKA is associated with less pain, reduced analgesia requirements and decreased reduction in post-operative haemoglobin levels. These short-term benefits are found to be of great value since they decrease the time of stay in the hospitals. In the era of value-based healthcare, providers and healthcare systems are concerned about any additional expenditures. As margins continue to decline, new expenditures must enhance the value of care provided.
When comparing the outcomes of the RTKA and MTKA, several studies have reported better short-term outcomes with RTKA. Marchand et al. published research in 2019 that reported a better mean pain score and functional score for RTKA compared with MTKA over one year6. Another prospective multi-centre study carried out in 2020 yielded similar outcomes. The patients were found to have large improvements in standing and walking, advanced activities, a better satisfaction score and a low score of pain on walking post 4 to 6 weeks after RTKA.
The results comparing the long-term outcomes have not been so straightforward. A study published in 2019 suggested that the prevalence of hip-knee-ankle angle outliers was 10.7% in the robot-assisted group and 16.5% in the conventional group (P =.172). In addition, there was no significant difference between the two groups regarding complications, including revision surgery7. Similarly, Eun-Kyoo et al. concluded that without differences in clinical assessments, robotic-assisted TKA appears to lower the frequency of mechanical axis alignment outliers and enhance the ability to achieve flexion-extension gap equilibrium. These studies were conducted on the first generation of robotic instruments, and further research needs to be carried out.
In conclusion, RTKA inarguably has been reported to have better short-term outcomes. The genuine concern arises from the high cost of this procedure compared with the MTKA. In time, this hurdle may be overcome with wide distribution of robotic units worldwide and familiarizing adequate surgeons and OR staff with the equipment. How long it will take remains to be seen. In the meantime, MTKA techniques are to be improved, giving patients greater satisfaction and a better mobility range.
Kinomatic is unique in that it combines both the benefits of RTKA with the benefits of MTKA when in the hands of exceptionally skilled surgeons. With an even greater amount preoperative planning completed for each surgery compared to robotic assisted surgeries, Kinomatic is able to provide surgical details that are unrivaled in the precision joint replacement space.
To learn more about Kinomatic Custom Surgical Planning head to our website, www.kinomatic.com
References:
- Hampp, Emily L., et al. “Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques.” The Journal of Knee Surgery 32.03 (2019): 239-250.
- Shalhoub, Sami, et al. “Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate post-operative ligament balance.” Arthroplasty today 5.3 (2019): 334-340.
- Kayani, Babar, et al. “Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system.” The Journal of arthroplasty 33.8 (2018): 2496-2501.
- Tompkins, Geoffrey S., et al. “Robotic versus manual total knee arthroplasty in high volume surgeons: a comparison of cost and quality metrics.” The Journal of arthroplasty 37.8 (2022): S782-S789.
- Sodhi, Nipun, et al. “The learning curve associated with robotic total knee arthroplasty.” The journal of knee surgery 31.01 (2018): 017-021.
- Marchand, Robert C., et al. “One-year patient outcomes for robotic-arm-assisted versus manual total knee arthroplasty.” The journal of knee surgery 32.11 (2019): 1063-1068.
- Jeon, Sang-Woo, Kang-Il Kim, and Sang Jun Song. “Robot-assisted total knee arthroplasty does not improve long-term clinical and radiologic outcomes.” The Journal of Arthroplasty 34.8 (2019): 1656-1661.