A Reliable New Anatomical Landmark for Predicting Femoral Anteversion Angle?
In the elderly population, proximal femur fractures account for many fatal fractures. Surgical intervention is the standard treatment for a proximal femur fracture1. Depending on the severity of the fracture and the surgeon’s preference, proximal femur fractures can be treated with either an intramedullary (IM) nail, an extramedullary sliding hip screw (SHS), or a hip arthroplasty procedure. This makes surgery of the proximal femur a fairly common procedure and one that needs to be done perfectly to the tiniest detail to enable the person to have good functional mobility post-procedure.
When undergoing surgery on the proximal femur, it is tantamount to be extra careful regarding the femoral neck-shaft angle and the femoral anteversion angle. Fixation of femoral neck fracture and slid capital femoral epiphysis with lag screws and pins requires attention to these angles. When doing a transtrochanteric rotational osteotomy for osteonecrosis, Perthes disease, or a severe case of slipping capital femoral epiphysis, femoral anteversion is a crucial factor in getting an acceptable postoperative intact region. In short, any surgery on the proximal femur is doomed to go down the drain if not enough focus is directed toward the femoral anteversion angle.
Different imaging modalities, such as fluoroscopy, radiography, ultrasound, magnetic resonance imaging (MRI), and computed tomography, have been used to determine the femoral anteversion angle (CT). CT is useful for portraying fully ossified bones because of its high contrast between bone and soft tissue. CT of the entire femur is ideal, but it is not always feasible due to patient age, pregnancy, radiation exposure2, hospital budget, and capacity to do the procedure. The perils don’t just end here. It often becomes difficult to do a CT scan of the entire femur due to the inappropriate position of the hip joints in people with osteoarthritis and a restricted range of motion.
This brings us to our point of discussion of what anatomical landmarks can be used to assess femoral anteversion angle accurately. Historically, the anteroposterior axis of the femur (Whiteside’s line), the anteroposterior axis of the tibia (Akagi’s line) and lesser trochanter lines have all been used to predict the femoral anteversion line. We discuss how the anterior wall of the greater trochanter can be used as an alternative anatomic landmark in predicting femoral anteversion angle.
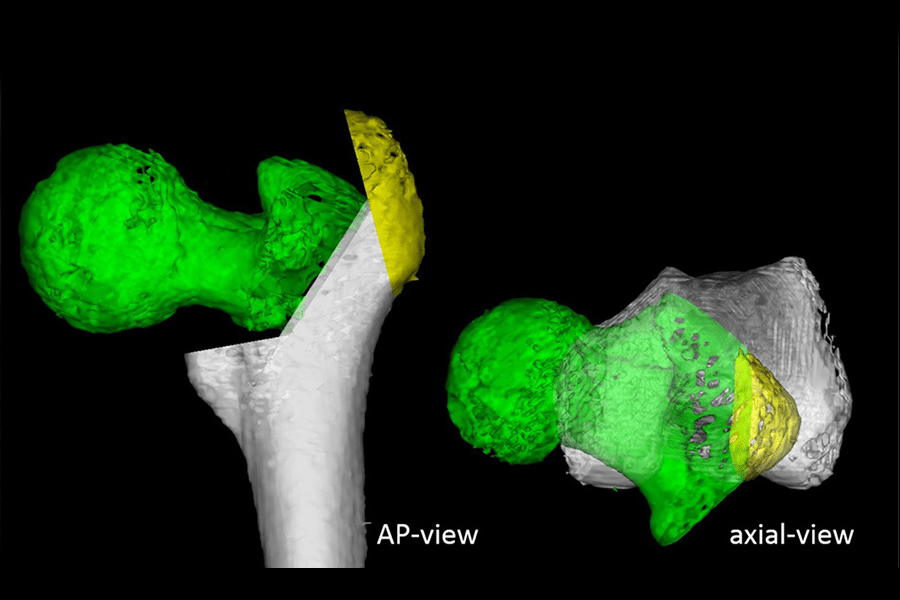
Before we get all excited and think of the greater trochanter as the next big thing to help us determine the femoral anteversion angle, we need to decide what exactly will be defined as the anterior wall of the greater trochanter. In this study published in 2022, once they had done the CT scan and reconstructed images with CT-based simulation software, they cut the greater trochanter through a point passing 5mm distal to the lateral ridge of the GT, giving a maximum thickness of 10 mm. The anterior wall of the cut surface was a flat line tangential to the anterior wall, defined as the anterior wall line3.
The results of the aforementioned study are pretty encouraging. Not only femoral anteversion angle is calculated without the absolute of the CT scan of the entire femur, but it can also be used when using the anterior approach, something that is a limitation while using the lesser trochanter line as the anatomical landmark since it can only be used when the proximal femur is approached posteriorly.
However, at the current point, putting forth a statement that the anterior wall of the greater trochanter should only be used will not be wise. The study described above has shown no patients with a proximal femur deformity or osteophyte formation. This way, it is very helpful for procedures involving the hip joint in young patients without deformity, such as the joint-preserving trans-trochanteric rotational osteotomy for osteonecrosis of the femoral head (ONFH) and internal fixation for femoral neck fracture and sliding capital femoral epiphysis. Unfortunately, patients with significant deformities of the proximal femur, such as those with end-stage osteoarthritis, osteonecrosis, and Perthes disease, may not benefit from using the anterior wall angle to forecast the femoral anteversion angle. Unfortunately, this study states that patients with significant deformities of the proximal femur, such as those with end-stage osteoarthritis, osteonecrosis, and Perthes disease, may not benefit from using the anterior wall angle to forecast the femoral anteversion angle.
Using this method clearly has its perks, and limited use of CT scan with simulation software has significantly reduced radiation exposure. However, plain radiographs would be perfect for predicting femoral anteversion.
To conclude, we have been introduced to a very workable anatomical landmark. Putting it into use has not only been statistically proven to be a real game changer but has also helped us halt unnecessary radiation exposure. Unfortunately, the answer to whether the anterior wall of the greater trochanter should be made the gold standard for predicting femoral anteversion will remain unchanged until we have extensive case series, new studies, and meta-analyses.
To read more about total joint arthroplasty go to www.kinomatic.com
References:
1. Hahnhaussen, Jens, et al. “High-energy proximal femur fractures in geriatric patients: a retrospective analysis of short-term complications and in-hospital mortality in 32 consecutive patients.” Geriatric Orthopaedic Surgery & Rehabilitation 2.5-6 (2011): 195-202.
2. Brambilla, Marco, et al. “Multinational data on cumulative radiation exposure of patients from recurrent radiological procedures: call for action.” European radiology 30.5 (2020): 2493-2501.
3. Suzuki, Masahiro, et al. “Utility of anterior wall of greater trochanter in predicting femoral anteversion angle: a three-dimensional computed tomography-based simulation study.” Journal of Orthopaedic Surgery and Research 17.1 (2022): 1-7.