The Goal of Knee Replacement
The goal of Knee replacement is to resurface the damaged cartilage in order to relieve pain and restore the alignment and function of your knee. Your doctor may recommend surgery if non-surgical treatment options have failed to relieve the symptoms.
Traditional knee replacement offers a cookie-cutter approach to surgery. With Kinomatic surgical planning, your surgeon can use a minimally invasive surgical approach and resurface the bone by removing just a few mm of bone. There are 3 bone surfaces that need to be resurfaced. Making sure that all 3 are aligned to fit you is no easy feat. Kinomatic surgical planning removes all uncertainty and helps your surgeon achieve the best possible outcome.
What makes Custom Knee Replacement Unique from Traditional Surgery
Taking the Guesswork out of Surgery
Custom Surgery allows your surgeon to know everything about your anatomy and your surgery in advance resulting in more accurate and efficient procedures.
Personalized to Best Fit your Unique Anatomy
We take countless measurements of your entire lower anatomy. This allows us to personally plan your knee replacement that’s going to feel like a natural joint.
Optimized Surgery for an Optimized Recovery
Because Kinomatic procedures involve less intraoperative guesswork, patients will typically experience less pain and get back to normal activity more quickly.
Knee Replacement by the Numbers
800K
Knee Replacements performed each year in the U.S.
3.5M
Projected knee replacements annually by the year 2030.
1 of 2
U.S. adults develop knee osteoarthritis in at least one knee in their lifetime.
80%
Knee replacements still functioning after 20 years.
Symptoms of Knee Pain
Swelling at the knee joint
Stiff knee joint
Knee is red or warmer than the surrounding tissue
Your knee makes popping or crunching sounds when in motion
You are unable to straighten your knee
Knee feels weak or unstable
Learn More About Knee Replacements
Navigate

The Knee Function
The knee is made up of the lower end of the thighbone (femur), the upper end of the shinbone (tibia), and the kneecap (patella). The ends of these three bones are covered with articular cartilage, a smooth substance that protects the bones and enables them to move easily within the joint.
The menisci are located between the femur and the tibia. These C-shaped wedges act as “shock absorbers” that cushion the joint. Large ligaments hold the femur and tibia together and provide stability. The long thigh muscles give the knee strength. All remaining surfaces of the knee are covered by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage, reducing friction to nearly zero in a healthy knee.
Normally, all of these components work in harmony, but disease or injury can disrupt this harmony, resulting in pain, muscle weakness, and reduced function.

What are the Common Causes of Knee Pain?
Knee pain can be the result of several conditions. An accurate diagnosis must be made to determine how to best treat your symptoms:
- ACL Injury
- MCL Sprain
- Dislocated Kneecap
- Bakers Cyst
Other Causes of Knee Pain
Chronic knee pain is commonly caused by arthritis. Arthritis is a term used to describe pain and inflammation in the joints. While there are many types of arthritis, the three most common types that lead to pain and loss of mobility are:
Osteoarthritis
According to the Centers for Disease Control and Prevention (CDC), osteoarthritis is the most common type of arthritis. Osteoarthritis (OA) is an age-related form of arthritis that causes joint pain and stiffness. As we age, the cartilage that cushions our joints begins to wear away, eventually leading to painful bone-on-bone contact. This type of arthritis is more common in people over 50 years of age, although it has been seen in younger patients. Osteoarthritis is the most chronic condition of the joints which affects approximately 27 million Americans.
Symptoms often develop slowly and tend to worsen over time. Typical signs and symptoms include: pain in your joints with movement, tenderness, stiffness, loss of flexibility limiting range of motion, and bone spurs (extra bits of bone which feel hard and can form around the joint). Common risk factors of osteoarthritis include: increasing age, obesity, previous injury, joint overuse, weak muscles, and genetics. There is no proven treatment for osteoarthritis. The most common way to help alleviate osteoarthritis is by physical measures, drug therapy, and surgery. Osteoarthritis was once believed to be just “wear and tear” on the joint as a natural part of aging. The condition is now viewed as a disease that attacks the joints in the body.
Several issues can contribute to the development of osteoarthritis in the knee joints, including:
Genetic Predisposition
Some genetic factors come into play, and it is believed that some people have a defect in the genetic code that directs collagen production in the body. Other patients may have inherited a minor flaw in how the knee joints fit together that leads to faster wearing of the cartilage.
Weight
When a person carries excess weight, it naturally places more stress on the weight-bearing joint at the knee. This causes the cushioning cartilage to wear away more quickly. It is believed by some researchers that the presence of excess fat in the body leads to the production of inflammatory chemicals that may damage the joint. A study published in the Journal of Orthopaedic Research found that losing just 5% of body weight can significantly reduce knee pain and improve function in people with knee osteoarthritis.
Injury, Excessive Knee Use
Some people have performed repetitive motions at work, in athletic pursuits, running, or other activity that eventually affects the function of the knee joint. Types of jobs that involve a great deal of time standing, lifting, or other similar activity can wear away the joint more rapidly. Injuries to joints such as damage from a fall, car accident, or other event can lead to a fracture which eventually leads to developing osteoarthritis.

Alignment and Kinematics of the Knee
The knee is often referred to as a “hinge” joint, however, this can be an oversimplified classification for the type of movement that the knee is capable of.
Hinge is typically termed as a mechanism to open and close doors, gates, and lids in one direction. Knee anatomy does allow for bending (flexion) and straightening (extension) in the sagittal (vertical, front to back plane) but the term “hinge” brushes over the complex range of motion the tibiofemoral joint allows for.
The knee has two semi-flat surfaces (plateaus) on the top of the tibial bone that articulate with round protrusions on the lower femur. This geometry allows for rotation, pivot, and gliding motion beyond just flexion and extension in the sagittal plane.
Anatomical knee kinetics can be seen in the egg-beater rotations of a water polo player or the pivots of a basketball player. Furthermore, the alignment of the knee is based on a mechanical axis running from the center of the ball and socket joint on the hip, down to the focal point of the ankle. If this line passes through the center of the knee then the patient has a neutral alignment. The line traced from the medial to the lateral side on the top of the tibia is known as the “joint line,” which is often tilted about 3° with respect to the mechanical axis. This means the tibial side of the joint has on average 3° of varus and the femoral end has 3° of valgus. Extreme varus and valgus alignments can lead to deformities.
A “valgus” knee consists of a joint collapsed medially inward (knock knee) or on the other extreme, bowed outward with a varus knee (bowlegged). 3D preoperative visualization can provide context to perform custom surgery catered to a deformity. Soft tissue ligaments and muscles are also integral factors in knee dynamics that can be altered in surgery or with postoperative physical therapy.
Physical therapy and exercise are essential components of the management of osteoarthritis. According to the American College of Rheumatology, regular exercise can improve joint flexibility, reduce pain, and increase muscle strength. Additionally, the use of assistive devices such as braces, canes, and splints can help relieve joint stress and improve mobility.

Types of Knee Replacements
Often pharmacological therapies such as non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and corticosteroids are used to mitigate the painful symptoms of osteoarthritis. Topical analgesics and joint injections may also be used to reduce pain and inflammation. However, these treatments only provide symptomatic relief and do not address the underlying cause of the disease. Tricompartmental knee replacement, also called total knee arthroplasty (TKA), is a surgical procedure in which the worn-out or damaged surfaces of the knee joint are removed and replaced with new parts. The knee is made up of the femur (thigh bone), the tibia (shin bone), and patella (kneecap). The meniscus, the soft cartilage between the femur and tibia, serves as a cushion and helps absorb shock during motion.
Arthritis (inflammation of the joints), injury, or other diseases of the joint can damage this protective layer of cartilage, causing extreme pain and difficulty in performing daily activities.
The knee can be divided into three compartments:
- Patellofemoral – The compartment behind the kneecap
- Medial compartment – The compartment on the inside of the knee
- Lateral compartment – The area on the outside of the knee joint
In a TKA the surgeon can choose between several techniques to realign the knee: Mechanical, Adjusted Mechanical, Kinematic, Restricted Kinematic, and Anatomical Alignment. The choice of technique is based on anatomy variation, and balancing soft tissue forces to create the best functional outcome. The alignments typically differ in the angles of cuts which result in varying axis alignment. In the procedure, the surgeon will make a cut across the superior surface of the tibia and the distal side of the femur to place metal tibial and femoral components. A plastic, typically polyethylene insert is placed between the two components to ideally mimic the natural capabilities of the joint. This is a fixed-bearing reconstruction which is common for a total knee replacement.
Partial Knee Replacement
Other options are also available for knee repair including partial knee replacement. Total knee replacements involve replacing the entire knee joint, while partial knee replacements involve only replacing the damaged portion of the knee joint. A study published in The Journal of Bone & Joint Surgery found that patients who underwent partial knee replacements had significantly lower rates of complications and shorter hospital stays than those who underwent total knee replacements.
However, partial knee replacements may not be appropriate for all patients with knee osteoarthritis, as they require a certain amount of healthy tissue in the knee joint to be preserved. Patients with advanced osteoarthritis that affects multiple parts of the knee joint may not be candidates for partial knee replacements.
Both partial knee replacements and total knee replacements can be effective surgical options for treating knee osteoarthritis. However, the choice between the two options should be made based on individual patient factors, surgeon guidance, and the extent of damage to the knee joint.
Bilateral Knee Replacement
A bilateral knee replacement means both knees are replaced at the same time. This might be recommended for patients who have significant damage in both knees. Although a bilateral knee replacement can be more complex than a single joint surgery, the benefits of bilateral total knee replacement can include a shorter overall recovery time, as well as the ability to return to normal activities more quickly. Physical therapy postoperatively can be more intense for a bilateral replacement because the patient must gain strength in both legs at the same time. However, the success of a bilateral replacement may be worth discussing with an orthopedic surgeon. Kinomatic offers a bilateral knee replacement option that only requires one CT scan and can provide additional accuracy preoperatively for a complex surgery.
Post-Op Knee Replacement & Physical Therapy
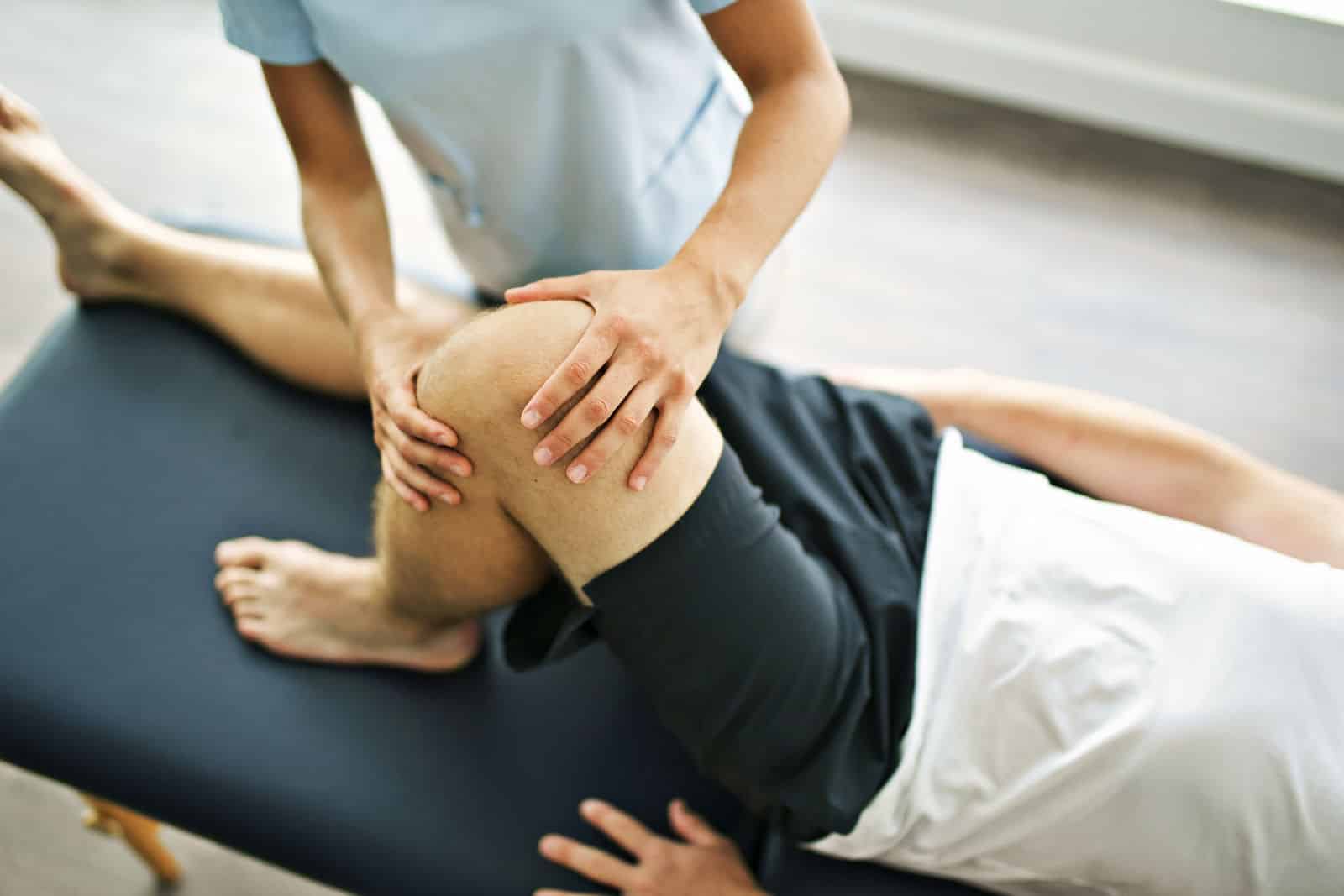
Rehabilitation after total knee replacement surgery is an important part of the recovery process, and physical therapy is a key component of this rehabilitation.
The goal of physical therapy is to help the patient regain strength, mobility, and function in the affected knee joint. In the early postoperative period, the focus is on reducing pain and swelling, as well as improving range of motion and muscle strength. The physical therapist will typically work with the patient to perform exercises to increase flexibility and strength, as well as teach techniques to help manage pain and prevent complications.
As the patient progresses in their recovery, the focus will shift to more functional exercises and activities, such as walking, climbing stairs, and returning to daily activities. The duration and intensity of physical therapy will depend on a variety of factors, including the patient’s age, overall health, and the extent of the knee condition. It is important for patients to be consistent with their physical therapy program, as this can help to ensure a successful recovery and improve overall outcomes.
Kinomatic utilizes OneStep’s physical therapy program to provide a custom total knee experience before and after surgery.